

Recent studies have examined the use of physostigmine in systemic inflammation, sepsis, and nerve gas exposure. Due to its increased side effects, medications with fewer side effects are preferable for the treatment of glaucoma. This increase results in increased aqueous humor flow and a decrease in intraocular pressure. The symptoms associated with anticholinergic toxicity are delirium, tachycardia, mydriasis, urinary retention, dry skin, and ileus.Ĭoncerning the treatment of glaucoma, physostigmine increases the levels of acetylcholine available for the ciliary muscle of the eye to contract. It is useful to treat the effects of anticholinergic toxicity on the central nervous system due to its ability to cross the blood-brain barrier. Physostigmine salicylate has FDA approval for use in treating glaucoma and the treatment of anticholinergic toxicity. From 1863 to this day, extensive research has been performed on the applications of physostigmine, examining its use in treating glaucoma to its use in the treatment of septic shock. Josef Pikl and Percy Lavon Julian synthesized physostigmine for the first time in 1935. A few decades later, in 1863, Sir Thomas Richard Fraser wrote his thesis on the medicinal uses of physostigmine. Although small in size, its lethality was first discovered by Sir Robert Christison in 1855. Physostigmine originates from the Calabar bean, widely found in the African tropics, and is a highly toxic parasympathomimetic alkaloid. If the poison is on the skin, then it must be washed off with soap and water.Physostigmine is a tertiary amine and a reversible cholinergic medication that was most commonly used to manage and treat antimuscarinic toxicity and glaucoma. If the substance enters the body through the respiratory system, you need to take the person to fresh air and rinse the nasal passages. The patient's stomach is washed with a solution of potassium permanganate and activated charcoal is given. If a person accidentally swallowed an organophosphorus substance, it is necessary to call a doctor as soon as possible and provide first aid to the victim. A severe condition called "cholinergic arousal" may develop with restlessness, delusions, and hallucinations. They can cause a drop in blood pressure, tachycardia, and impaired liver function. They are exclusively for hospital treatment of organophosphate poisoning.īoth remedies have severe side effects. These drugs can only be used in a hospital under supervision.doctor. They not only cannot be taken without the appointment of a specialist, but should not be used at home. A week later, cholinesterase activity doubles.įOS antidotes are strictly prescription drugs. Usually, 2-3 days after the start of therapy, enzymatic function begins to recover. During antidote therapy, it is necessary to control the level of cholinesterase activity. This can lead to the development of side effects and re-exacerbation of the symptoms of intoxication.
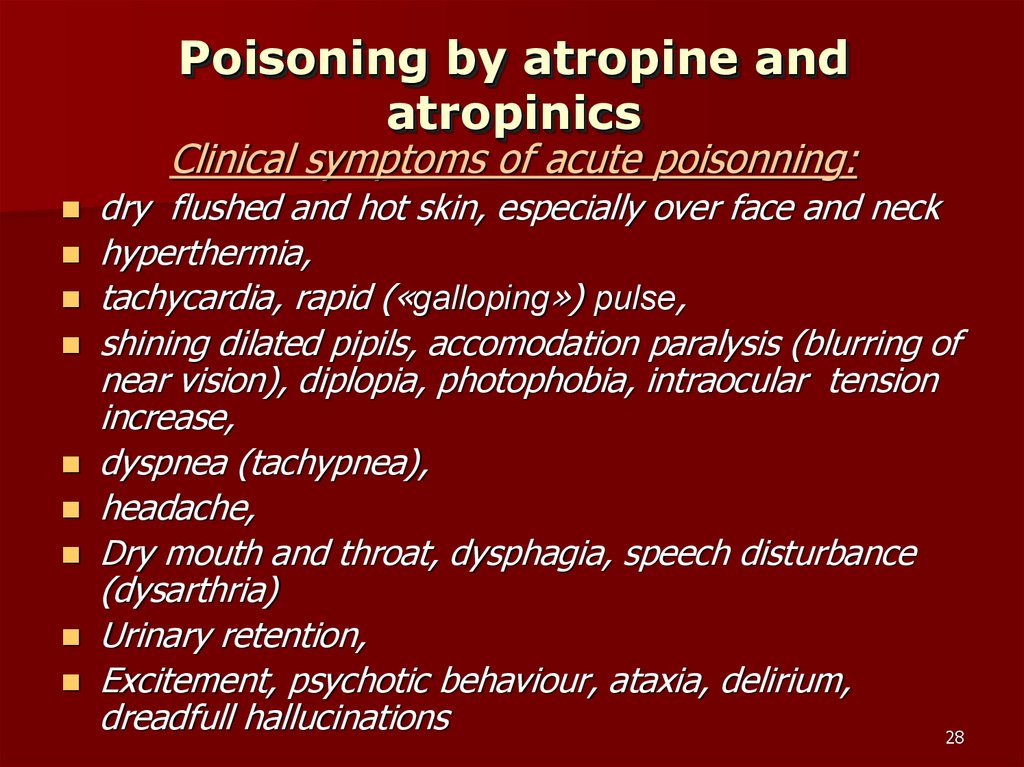
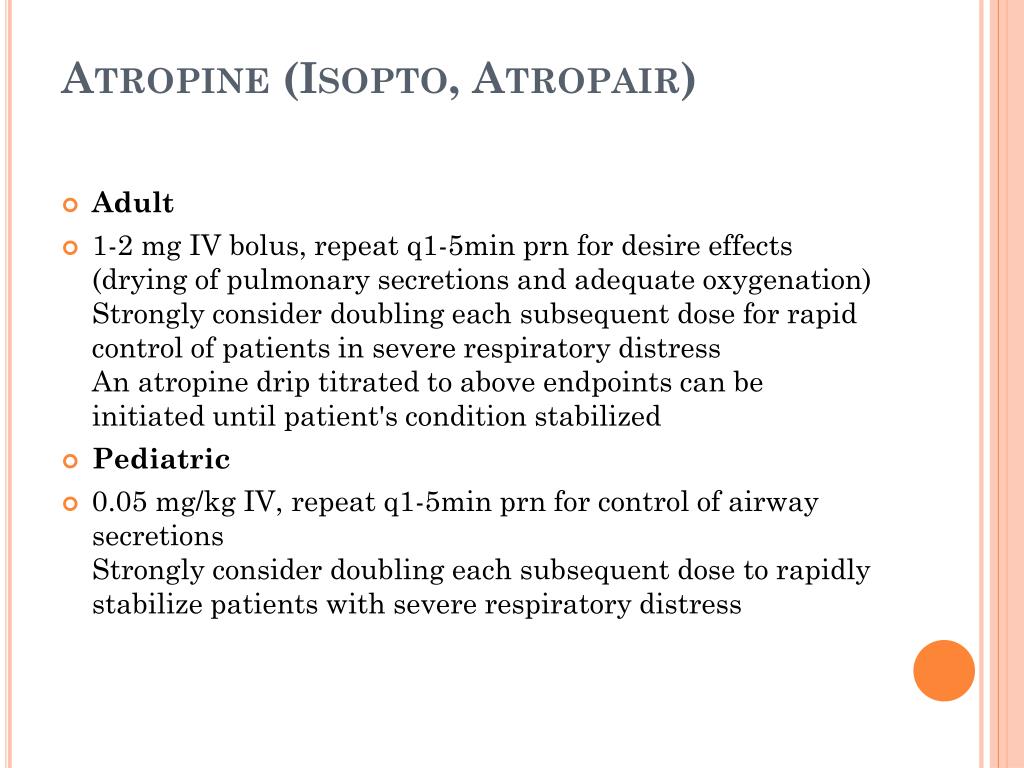
On the second day after poisoning, drugs are not administered. If necessary, enzyme reactivators are administered again.Ĭholinesterase reactivators mechanism of action These are signs of the effects of atropine on the body. Injections are stopped when dry mouth appears and pupils dilate. Atropine is administered every 5 minutes until wheezing disappears and the amount of mucus in the respiratory organs decreases. In severe poisoning, 3 ml of atropine and FOS antidotes are injected into a vein.If the manifestations of intoxication do not disappear, then the introduction of cholinesterase and atropine reactivators is repeated. At the initial signs of poisoning, 2-3 ml of atropine solution (0.1%) and FOS antidotes are injected under the skin, their dosage is determined by the instructions for use of each drug.


 0 kommentar(er)
0 kommentar(er)
